
Is excessive menstrual pain interfering with your life? 
Most women deal with the dull cramping pain (dysmenorrhea) in their lower abdomen during their period which can be quite unpleasant. However, about 10 percent of women have pain so excruciating every month it seriously hinders their daily lives.2 Menstrual cramps can actually be scientifically measured within the uterus, and the difference between mild and severe dysmenorrhea is considerable. The readings for normal periods are low pressure (50-80 mm HG) and can show 1-4 contractions every 10 minutes. A woman who has dysmenorrhea can produce readings of high pressure (over 400 mm HG) with contractions less than 15 seconds apart.5
Women can have two types of dysmenorrhea which have different underlying causes:
- Primary dysmenorrhea:? This period pain is the most common type and is not caused by any underlying disorder. It mostly affects adolescent girls and can start within six months to a year following the first occasion of menstruation. Primary dysmenorrhea can oftentimes be alleviated naturally with magnesium and calcium supplementation, and changes to lifestyle and dietary habits.
- Secondary dysmenorrhea:? Menstrual pain in this case is connected to some type of underlying medical condition (usually a disorder affecting the reproductive system) and can be relieved when the condition is treated. Secondary dysmenorrhea is most likely to develop in adulthood.2 Period pain is a common symptom of PCOS that can be considered to be an underlying condition, as well as endometriosis. If you have painful periods it’s an indication that it’s time to take action to heal your body.
+ Click here to learn about the all natural PCOS 5-Element Solution
+ Click here to read more articles about PCOS and Menstrual Irregularities
Causes
Most women get menstrual cramps during their period but why are yours so painful?
 Most women get menstrual cramps during their period but why are yours so painful? Period cramps (both mild and severe) are caused by the uterus contracting to help expel the uterine lining.5 This is a normal aspect of the menstrual cycle controlled by prostaglandins and other chemicals produced in the body. Dysmenorrhea becomes an issue when the level of prostaglandins is elevated.4 Severe uterine contractions can also constrict the blood vessels that feed your uterus, which produces pain comparable to angina resulting from blocked coronary arteries.3
Most women get menstrual cramps during their period but why are yours so painful? Period cramps (both mild and severe) are caused by the uterus contracting to help expel the uterine lining.5 This is a normal aspect of the menstrual cycle controlled by prostaglandins and other chemicals produced in the body. Dysmenorrhea becomes an issue when the level of prostaglandins is elevated.4 Severe uterine contractions can also constrict the blood vessels that feed your uterus, which produces pain comparable to angina resulting from blocked coronary arteries.3
Dysmenorrhea can be caused by different medical problems, such as endometriosis or PCOS, both of which can be treated to reduce the pain.
Your risk for painful periods also can be influenced by:3,4
- Irregular and heavy menstrual bleeding
- A poor diet
- Smoking
- Obesity
- Inactivity
- If you are younger than 20 years old
- Stress
- Family history of menstrual irregularities, including dysmenorrhea
- Inflammation
- Excessive levels of prostaglandins (the hormone that makes the uterus contract)
- Tilted uterus
Secondary dysmenorrhea can be caused by:2
- Adenomyosis
- Polycystic Ovarian Syndrome
 Fibroids
Fibroids- Tubo-ovarian abscess
- Ovarian torsion
- Sexually transmitted disease
- Cervical stenosis
- Ovarian tumor or cyst
- Pelvic inflammatory disease (PID)
- Intrauterine device (IUD)
- Endometriosis
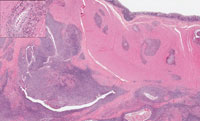
Painful periods can interfere with your daily life and many of the conditions that cause dysmenorrhea can cause serious health problems that can compromise your quality of life and fertility. Two common disorders that cause painful periods are endometriosis and Polycystic Ovarian Syndrome. Women who have endometriosis have cells that line the inside of the uterus implanting and growing outside it as well as on the bladder, fallopian tubes, bowels, and ovaries. Cells are not shed during menstruation because they are not in the uterus so pain occurs.6
Endometriosis can be mistaken for PCOS or can occur in addition to PCOS, but both are a result of hormone imbalance and inflammation.
Symptoms
How do you know if you have dysmenorrhea?
 The main symptom of dysmenorrhea is pain. This pain usually starts just before or at the onset of your period and lasts about three days, peaking at about 24 hours. Painful periods can be characterized by a dull deep ache or sharp knife-like cramps that can be felt in your lower abdomen and radiating to your hips, lower back, and even your thighs.4 You can also experience heavy bleeding and clots if your dysmenorrhea is associated with PCOS periods. Some women also experience dizziness, loose stools, vomiting, and sweating along with their period pain.3 If menstrual cramps impact your life negatively for several days a month or have just started being a serious concern, you should consult a doctor to rule out an underlying condition such as endometriosis.4
The main symptom of dysmenorrhea is pain. This pain usually starts just before or at the onset of your period and lasts about three days, peaking at about 24 hours. Painful periods can be characterized by a dull deep ache or sharp knife-like cramps that can be felt in your lower abdomen and radiating to your hips, lower back, and even your thighs.4 You can also experience heavy bleeding and clots if your dysmenorrhea is associated with PCOS periods. Some women also experience dizziness, loose stools, vomiting, and sweating along with their period pain.3 If menstrual cramps impact your life negatively for several days a month or have just started being a serious concern, you should consult a doctor to rule out an underlying condition such as endometriosis.4
Endometriosis and PCOS are common causes of painful periods but sometimes have very mild symptoms that don’t ring alarm bells. Both can cause serious damage, even infertility, if not treated.6 This is why it’s so important to be aware of the most common symptoms.
- Painful menstrual cramps that tend to worsen with time. As the growth associated with this disorder increases, each period the pain will increase also.
- Pain during intercourse
- Heavy periods over short menstrual cycles of less than 27 days
- Spotting in-between periods
- Continuous pain in the back or lower abdomen
- Fatigue
- Infertility
- Weight gain
- Facial hair growth or thinning hair
- Depression and anxiety
- Acne or dark skin patches
Endometriosis is often confused with PCOS, and women who have PCOS can also have endometriosis at the same time with overlapping symptoms.
Natural Therapies
What are some natural options for the treatment of painful PCOS periods?
Healthy diet choices, in particular, can provide a great deal of support for women with painful periods. Diets that are anti-inflammatory and lower in carbohydrates are a good start. A PCOS-friendly diet includes 100% grass fed meats, wild caught fish and seafood, eggs, berries, vegetables, and healthy fats. It is also a good idea to avoid caffeine, alcohol, hydrogenated fats, sunflower, safflower and corn oil, preservatives, and empty sugary calories. This type of diet will help regulate blood sugar levels and hormones leading to a more normal menstrual cycle.
A good diet is essential to managing painful periods. Focus on these foods to reduce inflammation and nourish your body:
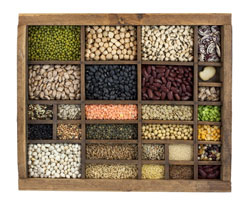 Healthy proteins: 100% grass fed meats, wild caught fish and shellfish, and organic cage-free eggs, legumes like lentils and other beans with nuts or seeds.
Healthy proteins: 100% grass fed meats, wild caught fish and shellfish, and organic cage-free eggs, legumes like lentils and other beans with nuts or seeds.- Healthy fats: avocado, coconut, nuts, seeds, olive, butter from 100% grass fed cows (pastured), ghee, grapeseed oil
- Healthy carbohydrates: vegetables of all kinds, lower glycemic fruits like berries, legumes, and gluten-free grains like quinoa or brown rice in small quantities.
Certain nutrients are beneficial in managing menstruation-related irregularities such as:

- Calcium and Magnesium: calcium can help to maintain muscle tone while magnesium helps to relax muscles. Sometimes this nutrient combination alone can alleviate symptoms.
- Flaxseed: This botanical assists with the symptoms of Polycystic Ovarian Syndrome by helping the body metabolize estrogen more effectively and increasing SHBG levels in the blood.1
- Stinging Nettle: Women with PCOS can sometimes have low levels of sex hormone- binding globulin (SHBG) in their blood, which can contribute significantly to the severity of menstrual issues like dysmenorrhea. The root of stinging nettle can help increase or normalize these levels.
- Chaste Tree Berry: This botanical is known to positively impact PCOS symptoms connected to hyperprolactinemia by helping to normalize prolactin levels. Chaste tree berry also helps normalize the hormones that are important during the luteal phase of the menstrual cycle.
- Vitamin E: This vitamin has been shown to be effective in improving primary dysmenorrhea when taken a couple of days before menstruation and a couple of days following the onset of your period. A good dose to consider is 500 mg/daily of mixed tocopherols.1
- Vitamin B12: combined with fish oil – This combination has been shown to help reduce the severity of painful periods.1
- Yarrow: This botanical can help minimize symptoms such as heavy or painful periods associated with endometriosis, ovarian cysts, and PCOS.
- The Insulite nutrient system contains many of these nutrients and gives a good foundation for addressing some of the underlying causes – learn more here
Here are some very effective non-medical therapies to relieve period pain:2
- Applying heat to your lower back and abdomen with a heating pad or hot water bottle
- An epsom salt bath using hot water (as hot as you can stand it), 2 cups epsom salt and 1 cup baking soda
- Mild exercise such as walking or yoga to improve blood flow
- Lying on your back with your knees elevated
- Gentle massage on the lower back or abdomen
- Avoiding stress
You can also consider alternative therapies such as acupuncture or hypnosis. Both have been found to help alleviate symptoms associated with the disorders.4
The Insulite 5-Element System for PCOS was designed specifically to manage the underlying causes of PCOS and hormone imbalance that can directly improve painful periods. The System teaches you how to use nutrients, food, and movement to feel better and has a cravings component that is beneficial for long-term healing.
Next Steps
- Take the PCOS Quiz! Get your score and assess your hormone health risks.
- Join our Facebook Sisterhood Group Pose your questions to this group of like-minded women. Get the answers to your questions and the support you need.
- Checkout the Hormone Reset. Guided Practices to eliminate anxiety, lose weight and boost energy.
We are committed to helping women reverse their symptoms of hormone imbalance – a major cause of excess weight gain, adult acne, unwanted facial hair, depression, anxiety, and heartbreaking female infertility.
©Insulite Health empowers women with hormone imbalance to transform their lives through a process of healing with the Natural Hormone Solution –a complete solution for helping women reverse the symptoms hormone imbalance..
